Faculty Expert: Virology Professor Troy Cline
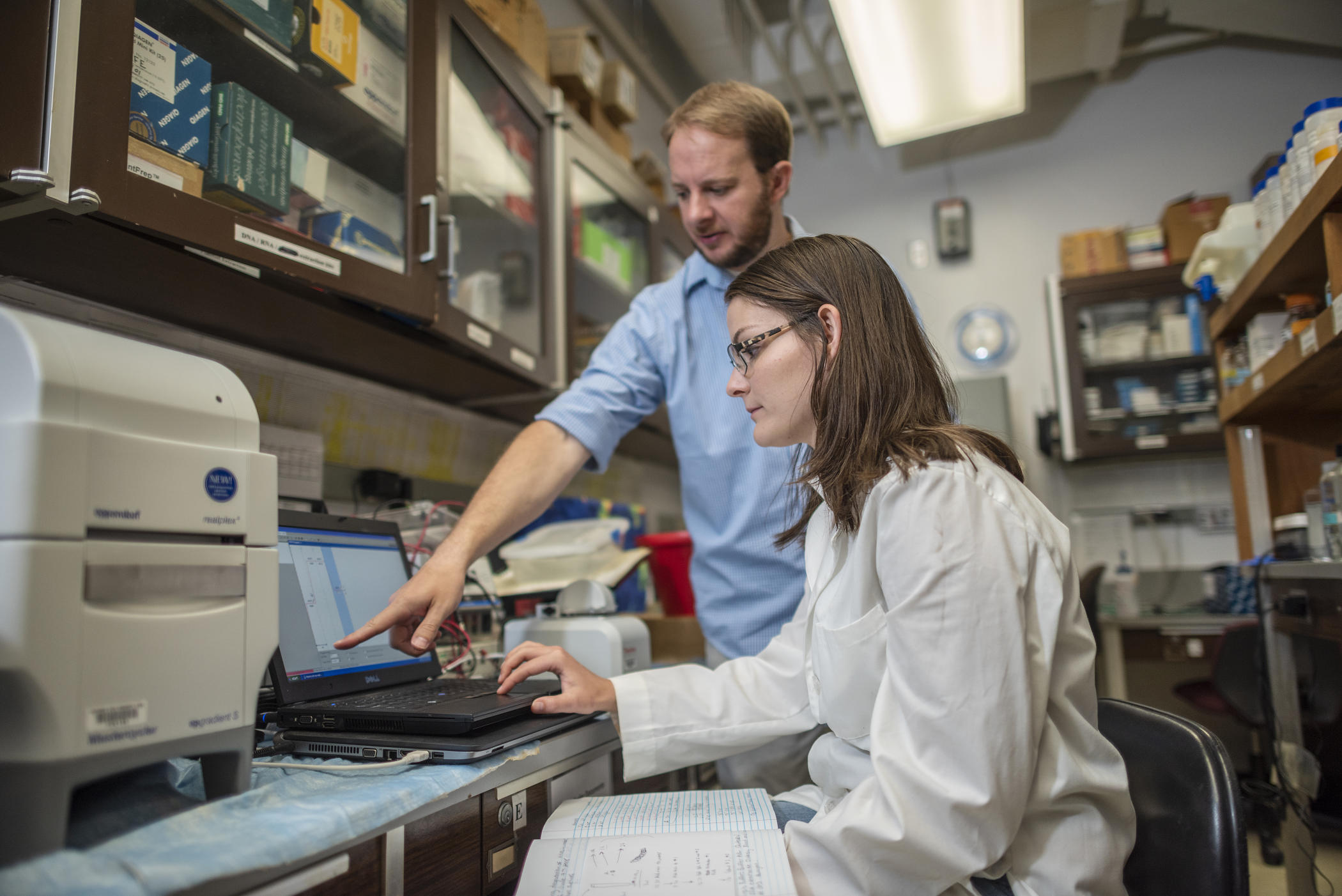
Faculty Troy Cline (left) works with Jessica Burris (right) on research about the role of feeding behavior on susceptibility of Northern Shovelers to Avian Influenza Virus infection as part of the Chico STEM Connections Collaborative (CSC2) Natural Sciences Undergraduate Research Project (UGR) on Thursday, July 5, 2018 in Chico, Calif. (Jason Halley/University Photographer/CSU Chico)
By Kacey Sycamore
Biological sciences professor Troy Cline teaches virology—or the study of viruses. So when the coronavirus pandemic emerged, his classes suddenly took on a real-world immediacy.
With a PhD from Ohio State University in viral immunology, Cline’s background is in studying immune responses to respiratory viral infections—in particular, influenza. We spoke with Cline about what stands out to him about the current novel coronavirus (COVID-19) spreading across the globe, and how he’s been incorporating the crisis into his lessons.
How much of your teaching has shifted to focus on what’s happening now?
All of it, literally. This is the [fifth] week of online courses, so for the [four] weeks after spring break and then Monday of this week, my virology class was just about coronaviruses, all aspects of coronaviruses. And then of course, focusing on the current pandemic, the public health response to it, the rationale behind the physical distancing, efforts to develop antiviral drugs and vaccines. It’s really been kind of cool.
From the beginning of the semester up until spring break, I focused the course on the broad general principles of virology. Now in real time, where we’ve got a pandemic happening, I’m able to apply what’s going on in the world in so many ways to these broad concepts that we had already talked about. It’s actually working out quite well as far as students meeting learning objectives and getting relevant content.
Is a pandemic on this scale something that, given your expertise, you saw coming?
This is something that virologists and scientists have seen coming for a long time. Nobody would have been able to predict exactly what that virus would be, exactly where it would come from, necessarily. But we know that these pandemics are going to happen.
You’re probably aware that this coronavirus originated in bats, as did the SARS coronavirus. When SARS first emerged in 2003, up to that time, the only human coronaviruses that were known were those that caused the common cold. So it was a little bit surprising to scientists that a coronavirus could emerge to cause severe disease. So people went looking for the origin of the SARS coronavirus. They found it in bats and then, looking back in the literature as early as 2013, there are papers of scientists calling the warning shots that we are at risk of another coronavirus pandemic.
I think some of the response we’re seeing implemented during this pandemic comes from past pandemics—the 2009 influenza pandemic, the 2003 SARS pandemic—and lessons learned.
What are some of those lessons?
I suspect that one of the reasons recommendations to practice physical distancing and shelter in place were implemented relatively rapidly for this pandemic—where we haven’t seen them before in this country—is because of our past experience. Pandemic H1N1 influenza was in 2009, and you can look in the medical literature in the years following—there are public health and medical professionals saying, “here are the things that we didn’t do right with pandemic influenza, these are the kinds of things that we need to do better the next time.” I think some of this response some people are seeing as perhaps excessive or extreme is actually helping the current situation. And these are being implemented because of things that we look at in retrospect and say, “We could have done better.”
Are there any big misconceptions you think people have about this virus?
That this is just a flu, which has also been propagated by public personalities and officials. And a lot of people even have misconceptions about flu—they think flu is just a cold, which is also not true. But while it’s true that influenza can cause deaths—it can cause up to about a half a million hospitalizations and averages about 30,000 deaths in the United States—we have a flu vaccine that offers protection to a large number of immunized people each year. Even if you’re not immunized, you probably have some protection from exposure to influenza virus in prior years. That helps to prevent the spread throughout the country and helps to temper the effects.
Nothing like that exists for this virus. Because there’s not a vaccine, and it hasn’t existed in the human population before, nobody’s protected through prior exposure. Even if the disease severity does not sound great with COVID-19, the whole global population is susceptible to it in theory, so it will spread very quickly. Without any pre-existing immunity, if half of the people in the United States were to become infected, that’s 1 million to 2 million deaths with just a 1 percent fatality rate.
How can social distancing affect the outcome of this virus?
You hear a lot that the physical distancing and social distancing that we’re doing is really, really extreme, because relatively few people have died from this compared to past outbreaks. When this is all finished and we get back to normal life, if we look back at the statistics, and we hit that 100,000 deaths number some public health officials and scientists have been saying is quite possible, as a percentage of our total population, that is quite small. There might be people that look at all of the economic hardship and personal difficulties that we went through who say, “Well, why did we do all that? Social distancing trashed our economy for something that wasn’t that severe.” But the number of deaths would be much, much worse if we didn’t do this.
We don’t get to do the control experiment, or go back in time and repeat this without the social distancing to see how bad it would be. But it is certainly having a great impact. You can see that by comparing this situation in California versus the situation in New York. California put shelter-in-place recommendations in place earlier, closed schools earlier than most other states. And while the situation is still ongoing—and it could always go for the worse—at the current level, I think what we’re seeing is evidence that things are working.
Kacey Sycamore works as a freelance writer, editor, and producer for public media organizations in Northern California. A Chico State journalism alum, she and her husband recently moved back to Chico to start a family.


